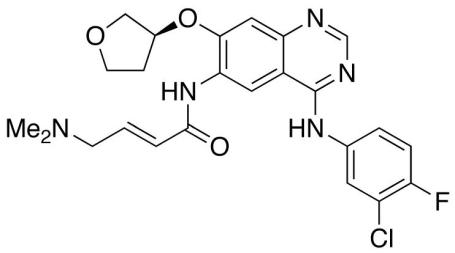
News reported by the Associated Press on July 12, 2013 is that the American Food and Drug Administration has approved the sale of Gilotrif (science name: Afatinib), made by Boehringer Ingelheim, used to treat about 10% of patients with non-small cell lung cancer (NSCLC)1.
But how does is this fabulous new drug work to help us live longer and treat one of the deadliest forms of cancer?
First off, Gilotrif is a small molecule compound developed by Boehringer Ingelheim chemists. It is designed to recognize and fit itself into a portion of a larger protein to prevent it from sending a message down the line. Think back to kindergarten and the exciting game of “telephone”. Imagine how hard it would be if something was designed to go over your mouth and prevent you from talking! Your ear still works and you can hear the message but you can’t pass it on! The game would end very quickly and the message wouldn’t be able to get down to the end of the line. This is exactly how this small molecule is designed to work.
Another important thing to know about this small molecule is just which protein it is designed to recognize and prevent from passing on a message. The protein family it inhibits is called the Epidermal Growth Factor Receptor (EGFR) family and they are normally found at the surface of cells and function by receiving signals from outside the cell and transmitting that message to the inside to initiate the growth and division of the cell which leads to the replenishment the epidermal tissue2. Epidermal tissue is the outer layer of tissue that separates the body from the outside world (skin, cells lining the exterior walls of the gut, and lungs). And from this information we can see that the cancers that this drug could potentially treat are limited to cancers that come from these tissues. Important to know; the originating cells of a cancer will mostly determine the overall lcharacteristics of the tumours.
So what is wrong with the EGFR family of proteins and why are they causing tumours?
Epidermal Growth Factor Receptors
(In case you were wondering, members of this family of receptors include the HER1, HER2, HER3, HER4 proteins.)
Normally, when these proteins receive an “it is time to grow and divide” signal from the outside, they relay that message to the inside of the cell through tyrosine-kinase activity. This is the scientific way of saying that this protein has the ability to add a flag (phosphate) to the amino acid tyrosine, found in many other proteins in the cell which starts a cascade of activity that eventually leads to the growth, survival and division of the cell.
However, in the case of cancer, the tyrosine kinase ability of the EGFR proteins have gained the ability to start the growth/division communication cascade within the cell without the need to recognize a signal from the outside of the cell. Think back to the game of telephone. This would be the same as one person in the game, without receiving a message, constantly passing on a message to their partner anyways. The whole game would be taken over by this message that was created by someone not following the rules! In cells, these unregulated messages can have profound, harmful consequences such as uncontrolled cell growth which can form a tumour mass.
So how does this protein become a rogue player in the game of telephone? A random mutation to this protein can cause it to send messages uncontrollably. These mutations often affect the “mouth” or tyrosine kinase sections of these proteins. Mutations can be caused by the usual cancer risk factors such as too much sun (UV rays), smoking, obesity, etc. There is also evidence that this mutated protein could be genetically linked. However, it is still not known if any real increase in cancer risk exists if you inherit these mutations (since there hasn’t been a study on this yet). But it is known that in most cases of non-smoking , non-risk factor associated lung cancers, this mutation can be found. On average this accounts for about 10-15% of lung cancers in Caucasian and about 50% of Asian patients2. This finding alone, suggests a possible link to genetics but it is not known for sure.
Benefits to blocking EGFR
Luckily for lung cancer patients, it has been found that in most EGFR mutated cases, the tumour growth and progression is completely dependent on EGFR signaling. That means if doctors and scientists can stop EGFR signaling then they can stop the growth of the tumours and stop cancer progression. They have done this in the past using tyrosine kinase inhibitors designed to plug up the “mouth” of the protein and prevent it from phosphate flagging the proteins in the cell. But the first generation of inhibitors used did not function as permanently as Gilotrif has been designed to. The older generation simply plugged the mouth but could easily fall out and EGFR would become active again. This new drug, Gilotrif, has been designed to plug up the mouth permanently by binding on very tightly to the tyrosine kinase site and never letting go. The only way for the cancer cells to grow again would be to make new EGFR and hope the drug Gilotrif is not present!
This is similar to plugging the mouth of a rogue telephone player and preventing them from passing on any message in the game.
Limitations and potential consequences
So as you could imagine, removing such an essential protein involved in the communication of epidermal cell replenishment could cause some problems. Common side effects are related to the fact that the cells in these tissues can not regenerate and make new tissue. Not replenishing gut cells results in stomach cramps, diarrhea, and nausea. Skin cells that do not grow can result in the formation of rashes, dry skin, and acne. And it has been reported that the incidence of side effects was quite high, upwards of 90% of treated patients2.
Another limitation highlights the resiliency of cancer and provides a micro-model of evolution at work. It has been reported from doctors that some cancers in patients receiving the first generation EGFR inhibitors can mutate further and continue to grow. This has been suggested to altering the tyrosine kinase area to prevent the first generation inhibitors from recognizing and plugging it up. This could also be a mutation that somehow bypasses the EGFR pathway and allows the cells to grow again. And just like evolution, if a mutation is beneficial to the survival of the cancer, these mutations are selected for and the cancer can continue to grow, resistant to first generation tyrosine kinase inhibitors. This resistance has also been detected in laboratory animal models of cancer receiving Gilotrif. This indicates that Gilotrif could cause these evolutions in a patient’s cancer as well.
Scientists and doctors hope to overcome this resistance by giving drug cocktails that target different pathways which support cancer growth. The hope is that by blocking multiple pathways, the cancer cells can’t gain all the required mutations at once to allow it to survive and continue to grow.
The development of this drug highlights the need to better understand cancer and hopefully future research can identify other cellular pathways crucial to the growth of cancer. That way, scientists and doctors can continue to develop drugs designed to specifically shut down these pathways and control the growth of cancer. Also, understanding the activity of the drugs allows improvements such as permanent binding to be made to upgrade our similar, existing drugs.
References
1) AP Staff; FDA approves drug to treat advanced lung cancer; July 12, 2013. (http://www.nbcnews.com/health/fda-approves-drug-treat-advanced-lung-cancer-6C10620068)
2) Valerie Nelson et al.; Afatinib: emerging next-generation tyrosine kinase inhibitor for NSCLC; OncoTargets and Therapy 2013; Issue 6 135–143.